Life on PICU is never boring; change comes by the hour, or the minute. The way in which Isaac adapts astounds me. For example, they gave him a suction and he's now commandeered this himself, regularly sucking the sputum from his mouth as he coughs it up, without giving it a second thought. What he can do himself, he does.
I know we've been in hospital six days now, but it feels a little shocking how ill he has become so quickly, it's still sinking in for us all. Today the physio had him up for a walk for the first time in days - about 15 yards to the door and back, for which he needed portable oxygen.
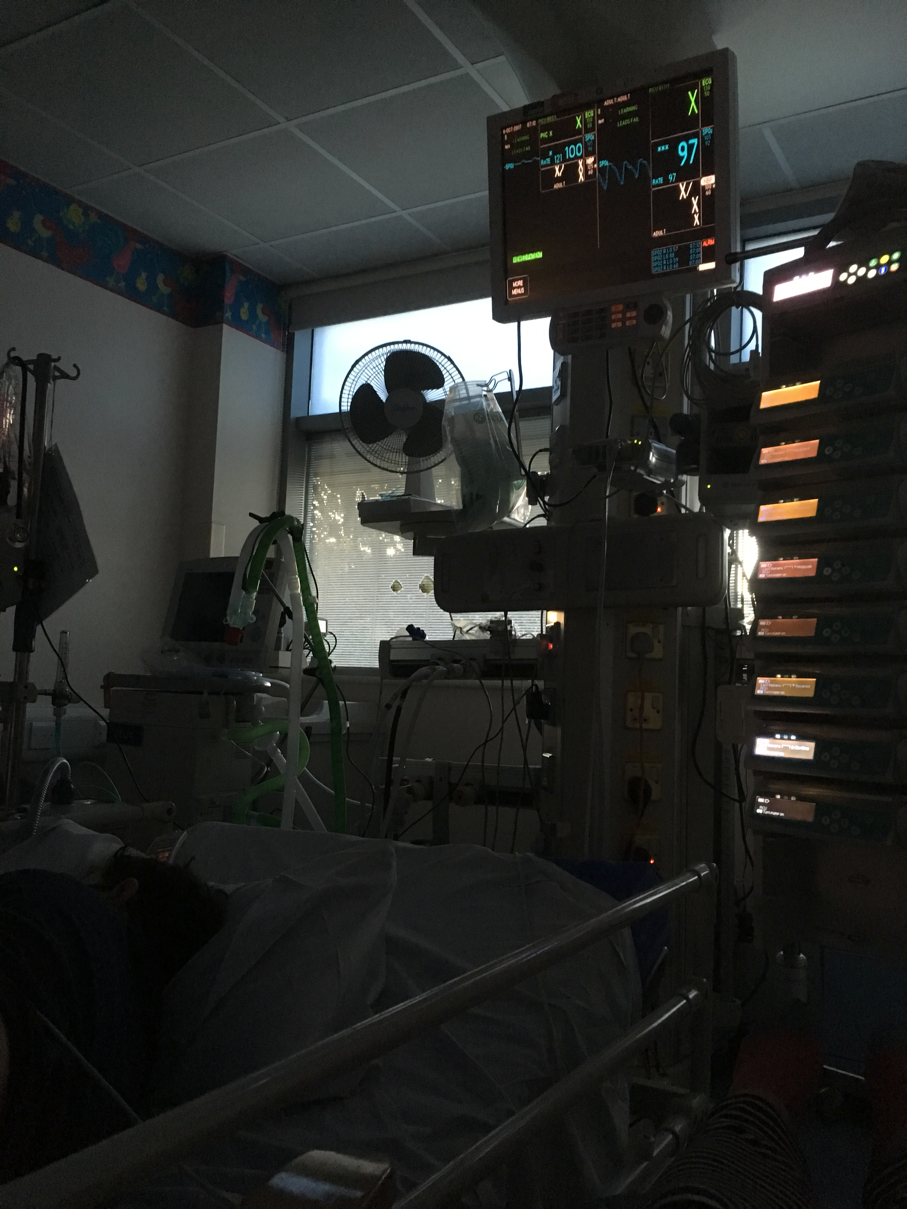
Back in bed, he remains on Opti-flow, on which we can increase and decrease either the flow (the force the air is given, to open up his airways) or the O2, depending on his sats. We aim for comfort and 94 and above. The wonderful nurses tweak things endlessly, making sure he is as comfortable as possible. He is eating very little. He has nebulisers pretty much hourly, along with his normal oral meds, 7 doses of IV antibiotics, and physio at least three times a day, so although he is sedentary, he is busy. Fuck, getting well can be hard work.
His cough remains as bad as when we came in. He can have a good 10-20 minutes, but then a coughing fit comes, and this can last just as long as the break that preceded it. It is violent, red faced, ferocious, and completely exhausting. Utterly heart wrenching to watch... but is is good, it is clearing his chest slowly. He is still being treated for assumed pseudomonas infection, which is a bug he is considered colonised with. They call this kind of infection flare up an exacerbation. He is not well enough for further lung function tests yet, but the tests he will have in the days, weeks, months to follow this will show what impact this exacerbation has had on his long term lung health.
Last night I came home to sleep with his sisters. Rosa is asking a lot of questions; why our family is never all home together, how we made sure she doesn't have CF, and why we didn't do the same for Isaac.... Anouk is very worried, and had a big cry with me. They came with me this morning when Dan and I swapped over, and saw Isaac for the first time in a few days. With the oxygen on his face, surrounded by machines, Rosa was too scared to hug him. This is huge for them too, but we try to make life as normal as we can, and the grandparents and family love and distract them as much as they can.
I am surviving on a diet of Diet Coke and brown bread and banana sandwiches; ideal as I don't need a fridge, and I can make them up with just a single plastic knife. Having a little more sleep helps a lot. Dan is brilliant.
Apologies for not replying to all messages, if I am repeating myself, or this is entirely nonsensical! Isaac had a funny moment yesterday, where he stuttered considerably, trying to say the word 'sure'. He looked at me, panicked, unsure why the messages whizzing round his brain would not let the word out. I understood exactly how he felt. Our minds are jumbled, our bodies tired.
I think tomorrow will be a better day.











 '
'