
A blog about Cystic Fibrosis, promoting organ donation, family, love, art, drinking too much tea (and quite possibly gin).
Monday, 30 July 2018
Hospital and hoping for holidays...

Saturday, 28 July 2018
Sick sick....


Tuesday, 24 July 2018
Cystic Fibrosis FAQs
What is a portacath? Isaac had a portacath surgically implanted in his chest wall earlier this year, the aim being easy venous access for regular IV treatment (IV being intravenous, as in, drugs delivered directly into his blood stream).
Regular cannula/long line/PICC line access over the years has wrecked his veins, and it became harder and harder to find a viable vein each time (veins repeatedly used would just collapse resulting in multiple needles, and often, delayed treatment when he needed it most). We had an agonising wait in HDU (high dependency unit) once, and delayed antibiotics give bugs a chance to fight back. Not good.
The port meant surgery, always advisable to avoid, but the hope is that this will last him 5-10 years before replacement. Cancer patients often have a port for for chemotherapy.
He still requires a needle to access it for use, but the key difference is trying to guide a line up a long, thin, windy and collapsible vein, usually blind (they can use ultrasound, but this is unusual) which often fails and needs repeated attempts, compared to a needle plopped right into a kind of rubber bung with a hole in the centre, and ta dah... you have accessed the (pre-accessed) vein.
What does having a port mean to Isaac? On the whole, it’s great. When his port is not accessed you can see only a smallish bump under his skin in his chest (with one scar nearby and a second by his neck, from the surgery). When it is accessed for treatment, he has a needle in for the whole course (usually 2-3 weeks at a time) and cannot get this wet, so no swimming or showers. The rest of the time, it’s life as normal, aside from avoiding full contact sports like rugby, which might damage the port.
In between treatments, the port is accessed every month for a flush to keep it clear. So it does still involve regular needles, but compared to cannulas, long lines and PICC lines, overall, it is a helluva lot less stabs!
What would a Transplant mean to Isaac? CF is a multi factor disease, it affects mainly his lungs, pancreas, liver, sinuses, and digestive system. A lung transplant would only cure the disease in his lungs. But this is also where the biggest risk to life is (90% of people with CF die from lung disease).
After transplant, people with CF no longer have CF lungs. However, infections in their sinuses may re-infect their lungs, meaning they need to carry on with some traditional CF lung treatments (but not all, and maybe very few).
Digestive health is unaffected by lung transplant, for example, Isaac will always need to take Creon in order to digest fats and proteins (pancreatic enzyme replacement meds, of which he takes about 50 capsules a day) and will continue to be at risk of CF related osteoporosis, diabetes, some cancers and liver disease.
Why not transplant now? You will hear me shout loudly on this blog about organ donation and the fact that we have chronic shortage of donors.
1 in 3 people on the waiting list for lungs dies waiting
I have often been asked why Isaac cannot be put forward for transplant now? The good news is; he is too well. The main test of wellness is a lung function test. His FEV (forced expiratory volume) is measured regularly and forms part of the picture on which his team plan his treatment. I don’t like to post much about his FEV, as I feel it becomes a focus on a number which is only part of a much bigger picture. Plus it fluctuates widely, at his worst (while in intensive care) he blew a 17%. Needless to say, his baseline is never as high as I would like it to be, but also, it’s not near the point where transplantation would be considered (regularly less than 30%).
More importantly, transplantation is not a cure; the chances of surviving the surgery for a year is only 80% and surviving 5 years 60%. This is a fast changing statistic, as development in anti-rejection therapies improve. Transplant is truly amazing, and life changing for many, but it’s also like swapping one disease for another, and further, a whole new set of not so fun side effects.
More FAQ’s to follow. Any questions, because medical jargon slips into my vocabulary pretty quickly, please do ask x
Wednesday, 11 July 2018
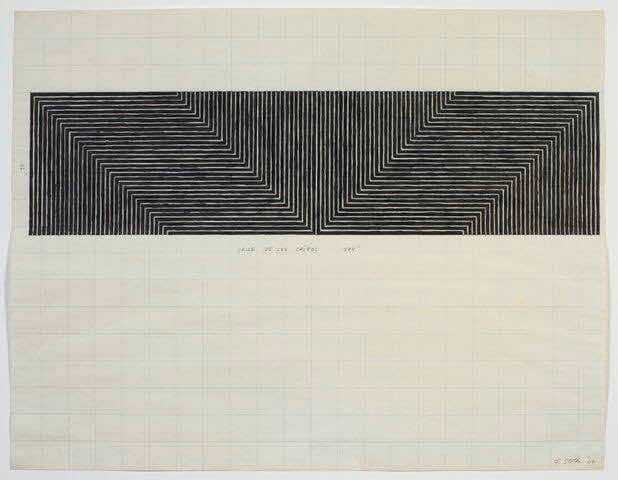
A squash and a squeeze


Thursday, 5 July 2018
NHS England deny Orkambi access
Sunday, 1 July 2018
Heat wave and wild woods






