Why Portacath? A portacath is an implanted venous access device for patients who need frequent or continuous administration of chemotherapy. Drugs used for chemotherapy are often toxic, and can damage skin, muscle tissue, and sometimes veins. They often need to be delivered into large central vein where the drugs are immediately diluted by blood stream and delivered efficiently to the entire body. Cancer patients also require frequent blood tests and scans to monitor their treatments. For patients with difficult veins, it can be used for withdrawing blood for blood tests, as well as diagnostic scans. Using modern techniques, the portacaths we have inserted are highly appreciated by patients, oncology nurses and doctors.
What is a portacath? A portacath consists of a reservoir (the port) and a tube (the catheter). The port is implanted under the skin in the upper chest. It may appear as a bump under the skin in thin patients, but less visible in patients with some subcutaneous fat. The catheter runs in a tunnel under the skin, going over the collarbone and then enters the large vein in the lower neck (the internal jugular vein). Since it is completely internal, swimming and bathing is not a problem. The septum of the port is made of a special self-sealing silicone rubber. It can be punctured up to one thousand times and therefore can be used for many years.
How is a portacath implanted? The procedure is performed under anaesthetic, with the aid of imaging guidance (ultrasound and X-ray) in the angiography suite of radiology department. The actual procedure takes about 30min. An intravenous sedation is given to make the local anaesthetic injection less painful. There will be a skin incision 3cm long on the chest wall for the port pocket and a 5mm nick in the lower neck to enter the vein. Absorbable sutures are used for the chest wound and are buried under the skin. For the small neck wound, sutures are usually not required and the wound is closed with Steristrips (medical sticky tape).
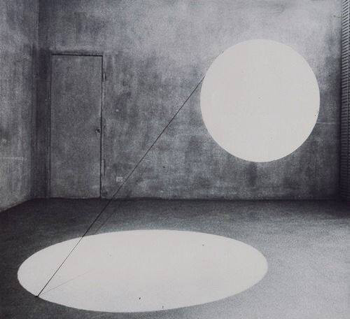
This is all taken from here (includes images) and while this references oncology patients, they are also very commonly used in CF for the same reasons. The end result, in his chest wall (when not accessed) will look something like this (only with less chest hair his case);
You can watch a video about how a port is then accessed for IVs here (basically, how a needle is stuck in to gain venous access). The needle then remains in for the duration of the antibiotic course (usually two weeks), in that time, he cannot bath (entirely), swim or do contact sports; but once the needle is removed, he can again. The skin just grows over the hole.
The reason Isaac is having a port fitted is because he now needs more regular IV treatment, and because his venous access is so poor; after years of IV antibiotics for two weeks at a time, blood tests, and other tests, his veins are, well, a bit shit. Don't worry, he has loads of other veins for blood delivery, only the ones we can use for intravenous access are now very limited. A port means an end to repeated attempts for peripharal lines (your average kind of cannula, usually in your hand or arm), long lines (usually in his arms or ankles) or PICC lines (usually in his arms, ankles, groin). Instead we will have a one-fits-all solution in his chest, which is great, but does come with all the usual risks of surgery, especially of infection (especially as this is so close to his heart).
As with any surgery, you don't exactly look forward to it, but in this case, we know it's the lesser of two evils.